A Divided Medical Community
The medical community has been divided for decades over the appropriate age to begin screening mammography for breast cancer and how frequently these mammograms should be performed. This division has been characterized by contrasting approaches, often labeled as “skeptics” and “interventionalists,” as detailed in Asia Friedman’s book Mammography Wars. Skeptics prioritize minimizing the potential harms of overdiagnosis and overtreatment, whereas interventionalists emphasize early detection to improve survival rates.
A Significant Development: New Guidelines
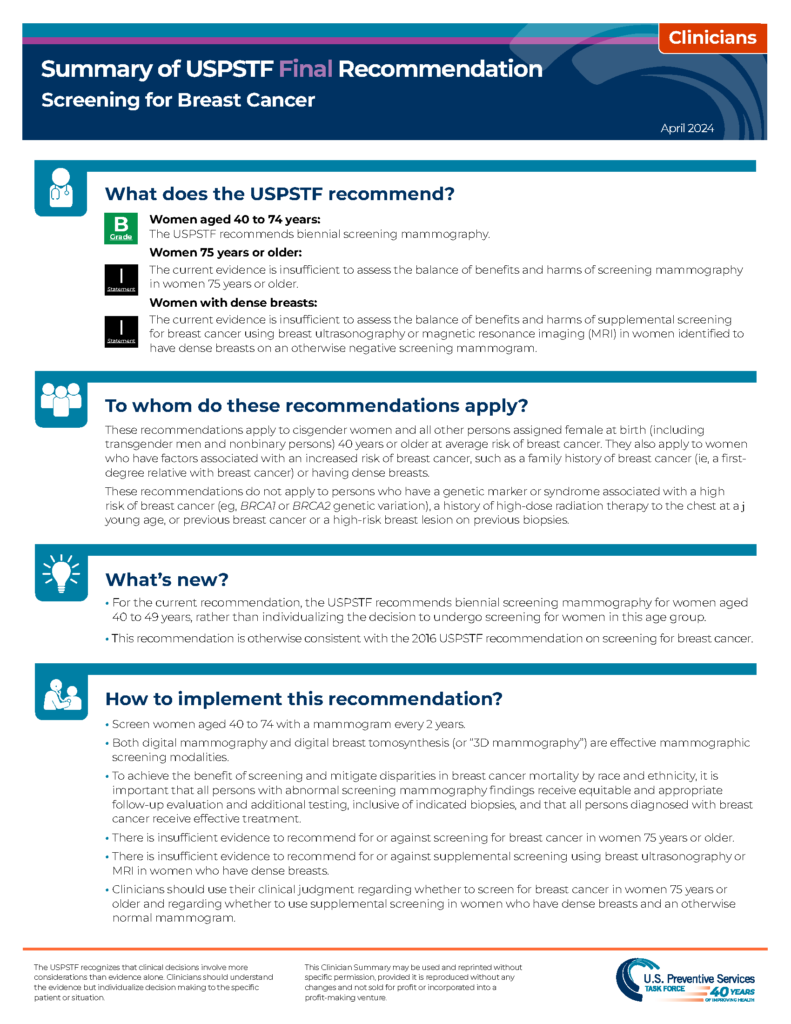
The U.S. Preventive Services Task Force (USPSTF) recently modified its breast screening recommendations. This modification has led to a consensus among the American Cancer Society (ACS), the American College of Radiology (ACR), and the National Comprehensive Cancer Network (NCCN) that screening mammography should commence at age 40.
The Impact of Evidence-Based Medicine
This alignment is a significant milestone and underscores the dynamic nature of evidence-based medicine and its ability to reshape healthcare recommendations for the betterment of public health. It highlights the delicate balance between avoiding the overuse of medical resources and ensuring that early detection does not miss potentially life-saving diagnoses. The agreement on the starting age for screening marks a milestone in prioritizing population-based guidelines and individual clinical experiences.
USPSTF’s Latest Guidelines
The USPSTF’s latest guidelines recommend that all women undergo biennial mammography starting at age 40 and continuing through age 74 to reduce mortality from breast cancer. This is a significant shift from the previous approach, which encouraged women in their 40s to make individualized decisions based on their health history and preferences. The new guidelines reflect a growing body of evidence suggesting that screening at age 40 can save more lives. This shift in policy underscores the importance of periodic reassessment of medical guidelines in light of new research and evidence.
Frequency of Screening: Points of Contention
The consensus among significant health organizations remains the same as the importance of individualized care. While the starting age for screening is now uniformly recommended, the annual or biennial frequency remains a point of contention. The American College of Radiology recommends annual screenings starting at age 40. The American Cancer Society, for example, recommends annual screenings for women aged 40 to 54, followed by biennial screenings for those 55 and older, while the USPSTF advises biennial screenings throughout. Despite these differences, the agreement on the initial age for screening represents a significant convergence of expert opinion.
Addressing Health Disparities
One of the critical aspects of the USPSTF’s recommendations is the call for more research to address health disparities in breast cancer screening and treatment. Women from Black, Hispanic, Latin, Asian, Pacific Islander, Native American, and Alaska Native communities often face unique challenges and disparities in healthcare access and outcomes. Black women, in particular, are 40% more likely to die from breast cancer than white women and are more prone to aggressive cancers at younger ages. Ensuring screening starts at age 40 is a crucial step but insufficient alone. There is an urgent need for more tailored screening strategies that can better serve these populations and improve equity in breast cancer outcomes.
Dense Breasts: A Special Consideration
Additionally, nearly half of all women have dense breasts, which can both increase the risk of breast cancer and reduce the effectiveness of mammograms. The Task Force acknowledges this issue and calls for more research on the benefits and harms of additional screening methods, such as ultrasound or MRI, for women with dense breasts. This highlights a broader challenge in medical practice: balancing population-based guidelines with individual variations in risk and response to screening.
The Role of Evidence-Based Medicine
The convergence of prominent health organizations on the starting age for breast cancer screening is a testament to the power of evidence-based medicine. Over the years, a wealth of research has contributed to our understanding of the benefits and harms of different screening strategies. Adapting and refining guidelines in response to new evidence is a hallmark of a robust healthcare system. This process enhances the quality of care and builds trust in medical recommendations among the public.
Integrating Research and Clinical Expertise
Evidence-based medicine plays a crucial role in navigating the complexities of healthcare decision-making. It allows for integrating clinical expertise, patient values, and the best available evidence. The recent alignment of screening guidelines exemplifies how continuous research and dialogue can lead to more effective and equitable healthcare practices.
A Significant Achievement
The agreement among major healthcare organizations to start breast cancer screening at age 40 represents a significant achievement in the ongoing effort to improve public health. Despite differing opinions on the frequency of screening, this consensus underscores the importance of evidence-based medicine in shaping healthcare policies. By balancing the need to avoid overdiagnosis with the imperative to detect cancers early, these guidelines reflect a nuanced approach to population health. Evidence-based medicine is a journey of continuous improvement, and this convergence in screening guidelines is a step forward.
Continuing the Journey
As we celebrate this milestone, we must continue advocating for research and policies that ensure all women receive the care they need to live longer, healthier lives. It is vital to heed the call for more research to address health disparities and improve screening for women with dense breasts, highlighting the ongoing commitment to refining and enhancing healthcare recommendations.
References.
Friedman, A. (2023). Mammography wars: Analyzing attention in cultural and medical disputes. Rutgers University Press. Nachtigal, E., LoConte, N. K., Kerch, S., Zhang, X., & Parkes, A. (2020, September). Variation in breast cancer screening recommendations by Primary Care Providers surveyed in Wisconsin. Journal of general internal medicine. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC7459047/
US Preventive Services Taskforce. (2024, April 30). Breast cancer: Screening. Recommendation: Breast Cancer: Screening | United States Preventive Services Taskforce. http://www.uspreventiveservicestaskforce.org/uspstf/recommendation/breast-cancer-screening

